Custom Search
Showing posts with label RADIOLOGY. Show all posts
Showing posts with label RADIOLOGY. Show all posts
5 Steps to Chest X-ray Interpretation
The video shows some basics of chest x-ray interpretation. From ed4nurses.com
Madelung's Disease (benign symmetric lipomatosis)
A 45-year-old man presented with a 3-year history of a painless, soft, and slow-growing swelling of the neck, upper trunk, upper back, and shoulders (Panels A and B). The patient had a history of heavy alcohol consumption and was a nonsmoker. Laboratory blood analysis showed minor elevations in aspartate aminotransferase (71 U per liter), alanine aminotransferase (49 U per liter), and total cholesterol (235 mg per deciliter [6.08 mmol per liter]). Triglycerides were very elevated at 1020 mg per deciliter (11.52 mmol per liter).
Magnetic resonance imaging revealed diffuse, nonencapsulated fatty deposits in the mediastinum and in the subcutaneous and deeper fascial compartments of the neck, upper trunk, and back (Panel C, arrows). A clinical diagnosis of Madelung's disease was made.
Madelung's disease (also known as benign symmetric lipomatosis, the Launois–Bensaude syndrome, and multiple symmetric lipomatosis) is a rare disorder of unknown cause. In reported case series, up to 90% of patients have a history of chronic alcoholism, and there is a strong male predominance. Since the patient was asymptomatic, no surgical treatment was proposed. He was started on lipid-lowering therapy and referred to an alcohol detoxification program.
Magnetic resonance imaging revealed diffuse, nonencapsulated fatty deposits in the mediastinum and in the subcutaneous and deeper fascial compartments of the neck, upper trunk, and back (Panel C, arrows). A clinical diagnosis of Madelung's disease was made.
Madelung's disease (also known as benign symmetric lipomatosis, the Launois–Bensaude syndrome, and multiple symmetric lipomatosis) is a rare disorder of unknown cause. In reported case series, up to 90% of patients have a history of chronic alcoholism, and there is a strong male predominance. Since the patient was asymptomatic, no surgical treatment was proposed. He was started on lipid-lowering therapy and referred to an alcohol detoxification program.
What is Periosteal reaction? it`s types? And how it is helpful in diagnosis.
 Periosteal reaction:
Periosteal reaction: A periosteal reaction is a non-specific reaction and will occur whenever the periosteum is irritated by a malignant tumor, benign tumor, infection or trauma.
There are two patterns of periosteal reaction: a benign and an aggressive type.
The benign type is seen in benign lesions such as benign tumors and following trauma.
An aggressive type is seen in malignant tumors, but also in benign lesions with aggressive behavior, such as infections and eosinophilic granuloma.
Benign periosteal reaction
Detecting a benign periosteal reaction may be very helpful, since malignant lesions never cause a benign periosteal reaction.
A benign type of periosteal reaction is a thick, wavy and uniform callus formation resulting from chronic irritation.
In the case of benign, slowly growing lesions, the periosteum has time to lay down thick new bone and remodel it into a more normal-appearing cortex.

Aggressive periosteal reaction
This type of periostitis is multilayered, lamellated or demonstrates bone formation perpendicular to the cortical bone.
It may be spiculated and interrupted - sometimes there is a Codman's triangle.
A Codman's triangle refers to an elevation of the periosteum away from the cortex, forming an angle where the elevated periosteum and bone come together.
In aggressive periostitis the periosteum does not have time to consolidate.

In these X-Rays:
* left:
Osteosarcoma with interrupted periosteal rection and Codman's triangle proximally.
There is periosteal bone formation perpendicular to the cortical bone and extensive bony matrix formation by the tumor itself.
* middle:
Ewing sarcoma with lamellated and focally interrupted periosteal reaction. (blue arrows)
* right:
Infection with a multilayered periosteal reaction.
Notice that the periostitis is aggressive, but not as aggressive as in the other two cases.
Note that:
They will not present with a periosteal reaction unless there is a fracture.
If no fracture is present, these bone tumors can be excluded.
So, Periosteal reaction excludes the diagnosis of Fibrous dysplasia, Enchondroma, NOF and SBC unless there is a fracture
Bronchiectasis in High-Resolution CT
Bronchiectasis is defined as localized, irreversible dilatation of part of the bronchial tree. Involved bronchi are dilated, inflamed, and easily collapsible, resulting in airflow obstruction and impaired clearance of secretions. Bronchiectasis is associated with a wide range of disorders, but it usually results from necrotizing bacterial infections, such as infections caused by the Staphylococcus or Klebsiella species or Bordetella pertussis.
Diagnosis of bronchiectasis is based on a clinical history of daily viscid sputum production and characteristic computed tomography (CT) scan findings.
Chest radiography is usually the first imaging examination, but the findings are often nonspecific and the images may appear normal. High-resolution computed tomography (HRCT) scanning has become the imaging modality of choice for demonstrating or ruling out bronchiectasis and its extent.HRCT scanning also helps clinicians to evaluate the status of the surrounding lung tissue and exclude other lesions such as neoplasms.
This is a Transverse high-resolution CT scans obtained in a 40-year-old man with bronchiectasis. (a) Scan shows small-airway disease denoted by centrilobular and tree-in-bud (black arrows) opacities and bronchiolectasis in the left upper lobe. Bronchiectasis in the upper lobe was assigned a grade of 1, with grade 1 (white arrows) bronchial wall thickening. In the apical segments of the lower lobes, grade 2 (arrowheads) bronchial wall thickening also is present. (b) Scan shows a combination of grade 1 (arrows) and 2 (arrowheads) bronchial wall thickening in the basal segments of the lower lobes with an overall bronchial wall thickening score of 1.5. The extent of bronchiectasis was evaluated as grade 3 in the right lower lobe and grade 2 in the left lower lobe. (c) Scan shows mosaic attenuation in both upper lobes. (d) Expiratory scan shows air trapping. The hypoattenuating areas (∗) were confirmed to be caused by air trapping in d.
Diagnosis of bronchiectasis is based on a clinical history of daily viscid sputum production and characteristic computed tomography (CT) scan findings.
Chest radiography is usually the first imaging examination, but the findings are often nonspecific and the images may appear normal. High-resolution computed tomography (HRCT) scanning has become the imaging modality of choice for demonstrating or ruling out bronchiectasis and its extent.HRCT scanning also helps clinicians to evaluate the status of the surrounding lung tissue and exclude other lesions such as neoplasms.
This is a Transverse high-resolution CT scans obtained in a 40-year-old man with bronchiectasis. (a) Scan shows small-airway disease denoted by centrilobular and tree-in-bud (black arrows) opacities and bronchiolectasis in the left upper lobe. Bronchiectasis in the upper lobe was assigned a grade of 1, with grade 1 (white arrows) bronchial wall thickening. In the apical segments of the lower lobes, grade 2 (arrowheads) bronchial wall thickening also is present. (b) Scan shows a combination of grade 1 (arrows) and 2 (arrowheads) bronchial wall thickening in the basal segments of the lower lobes with an overall bronchial wall thickening score of 1.5. The extent of bronchiectasis was evaluated as grade 3 in the right lower lobe and grade 2 in the left lower lobe. (c) Scan shows mosaic attenuation in both upper lobes. (d) Expiratory scan shows air trapping. The hypoattenuating areas (∗) were confirmed to be caused by air trapping in d.
To know grades of bronchial wall thickening:
Indications for OPG requests
An OPG or "ORTHOPANTOGRAM", gives a panoramic view of the mandible and teeth.
It is performed using a technique called "tomography". The X-ray tube moves around the head, the x-ray film moves in the opposite direction behind your head. This generates an image slice where the mandible and teeth are in focus, and the other structures are blurred.
* Peridontioiditis - when inflammation extends into the underlying alveolar bone and there is a loss of attachment.
* Peridontal Abscess - Radiolucent area surrounding the roots of the teeth.
* Panoramic view of mandible to view the fracture.
* Determine site and direction of fracture lines.
* Relationship of teeth to fracture lines.
* Alignment of bone fragments after healing.
* Evidence of infection or other complications post intervention.
* Follow up to assess healing.
* Patients on steriods after a transplant are immunosuppressed and the mouth is a common site of infection.
It is performed using a technique called "tomography". The X-ray tube moves around the head, the x-ray film moves in the opposite direction behind your head. This generates an image slice where the mandible and teeth are in focus, and the other structures are blurred.
Why to get it ?
Dental Disease
* Caries - appear as different shaped areas of radiolucency in the crowns or necks of teeth.* Peridontioiditis - when inflammation extends into the underlying alveolar bone and there is a loss of attachment.
* Peridontal Abscess - Radiolucent area surrounding the roots of the teeth.
Extraction of teeth (eg. wisdom teeth)
* OPG shows angulation, shape of roots, size and shape of crown, effect on other teeth.Teeth Abnormalities
* Eg. Developmental, to show size, number, shape and position.Trauma to teeth and facial skeleton
* Mandible fractures are often bilateral.* Panoramic view of mandible to view the fracture.
* Determine site and direction of fracture lines.
* Relationship of teeth to fracture lines.
* Alignment of bone fragments after healing.
* Evidence of infection or other complications post intervention.
* Follow up to assess healing.
Transplant workup
* To look for evidence of any underlying dental disease (eg. abscess)* Patients on steriods after a transplant are immunosuppressed and the mouth is a common site of infection.
Pneumocephalus
X-ray showing nasal and orbital fractures and pneumocephalus
Pneumocephalus is the presence of air in the cranial vault. It is usually associated with neurosurgery, barotrauma, basilar skull fractures, sinus fractures, nasopharyngeal tumor invasion and meningitis.Headache and altered consciousness are the most common symptoms.Tension pneumocephalus can occur and is a neurosurgical emergency.Plain X-rays can diagnose pneumocephalus, but CT scan is the diagnostic modality of choice.A classical CT sign of tension pneumocephalus is the “Mount Fuji sign”: the massive accumulation of air that separates and compresses both frontal lobes and mimics the profile of the large volcano in Japan.
Large right pneumocephalus compressing right frontal lobe and widening interhemispheric space. There are also air bubbles in basal cisterns and cerebellar fissures bilaterally
Most cases of pneumocephalus resolve spontaneously, and conservative management should be provided. Nonoperative management involves oxygen therapy, keeping the head of the bed elevated, prophylactic antimicrobial therapy (especially in post-traumatic cases), analgesia, frequent neurologic checks and repeated CT scans.
Supraspinatus Pathology by Ultrasound
This video details the complex structures of the human shoulder and how proper and careful ultrasound scanning techniques can identify tendon and rotator cuff tears, as well as avoid false positive and false negative tear diagnoses.
Contraindications to MRI procedure
The principal contraindications of the MRI procedure are mostly related to the presence of metallic implants in a patient. The risks of MRI scans increase with the used field strength. In general, implants are becoming increasingly MR safe and an individual evaluation is carried out for each case.
# Intra-orbital metal fragments
# Any electrically, magnetically or mechanically activated implants (including cardiac pacemakers, biostimulators, neurostimulators, cochlear implants, and hearing aids).
-other pacemakers, e.g. for the carotid sinus
-insulin pumps and nerve stimulators
-lead wires or similar wires (MRI Safety risk)
-prosthetic heart valves (in high fields, if dehiscence is suspected)
-haemostatic clips (body)
-non-ferromagnetic stapedial implants
Absolute Contraindications for the MRI scan:
# Intracranial aneurysm clips (Unless the referring physician is certain that it is made of nonferromagnetic material such as titanium).# Intra-orbital metal fragments
# Any electrically, magnetically or mechanically activated implants (including cardiac pacemakers, biostimulators, neurostimulators, cochlear implants, and hearing aids).
Relative Contraindications for the MRI scan:
-cochlear implants-other pacemakers, e.g. for the carotid sinus
-insulin pumps and nerve stimulators
-lead wires or similar wires (MRI Safety risk)
-prosthetic heart valves (in high fields, if dehiscence is suspected)
-haemostatic clips (body)
-non-ferromagnetic stapedial implants
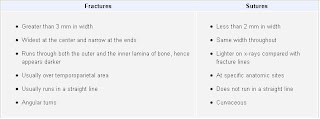
Differences between sutures and fractures in skull x-ray
Linear fracture results from low-energy blunt trauma over a wide surface area of the skull. It runs through the entire thickness of the bone and, by itself, is of little significance except when it runs through a vascular channel, venous sinus groove, or a suture. In these situations, it may cause epidural hematoma, venous sinus thrombosis and occlusion, and sutural diastasis, respectively. Differences between sutures and fractures are summarized in this Table
Click here for enlargment
Nutcracker phenomenon
It results most commonly from the compression of the left renal vein between the abdominal aorta (AA) and superior mesenteric artery (SMA), although other variants exist. The name derives from the fact that, in the sagittal view, the SMA and AA (with some imagination) appear to be a nutcracker crushing a nut (the renal vein).
There is a wide spectrum of clinical presentations and diagnostic criteria are not well defined resulting in frequently delayed or incorrect diagnosis. This condition is not to be confused with superior mesenteric artery syndrome, which is the compression of the third portion of the duodenum by the SMA and the AA.
This Computed tomography for a 52-year-old woman with mild episodic gross hematuria revealed compression of the left renal vein between the superior mesenteric artery (SMA) and the aorta (Ao) before the vein merges into the inferior vena cava (IVC). This compression caused marked dilatation of the distal part of the renal vein (RV). The renal venous congestion caused hematuria, presumably through the rupture of submucosal veins into the renal pelvis. No treatment was given. Entrapment of the renal vein is a known cause of hematuria.
There is a wide spectrum of clinical presentations and diagnostic criteria are not well defined resulting in frequently delayed or incorrect diagnosis. This condition is not to be confused with superior mesenteric artery syndrome, which is the compression of the third portion of the duodenum by the SMA and the AA.
This Computed tomography for a 52-year-old woman with mild episodic gross hematuria revealed compression of the left renal vein between the superior mesenteric artery (SMA) and the aorta (Ao) before the vein merges into the inferior vena cava (IVC). This compression caused marked dilatation of the distal part of the renal vein (RV). The renal venous congestion caused hematuria, presumably through the rupture of submucosal veins into the renal pelvis. No treatment was given. Entrapment of the renal vein is a known cause of hematuria.
Testicular microliths in a new born
The above ulltrasound images and Color Doppler image show testicular microliths (left testis) in a new born baby.
Testicular calcifications can occur in any age group; however the occurrence of this condition in a newborn is very rare. The color Doppler study showed normal vascularity in the affected testis.
Such cases need to be followed up for changes such as germ cell tumor and more benign conditions such as epididymitis, orchitis and varicocele as well as testicular atrophy. Studies show possible link between Testicular microlithiasis in infants and Down's syndrome.
Osteoporosis of aging (senile or postmenopausal osteoporosis)
Most common form of generalized osteoporosis. As a person ages, the bones lose density and become more brittle, fracturing more easily and healing more slowly. Many elderly persons are also less active and have poor diets that are deficient in protein. Females are affected more often and more severely than males, as postmenopausal women have deficient gonadal hormone levels and decreased osteoblastic activity.
Osteoporosis of aging. Generalized demineralization of the spine in a postmenopausal woman. The cortex appears as a thin line that is relatively dense and prominent (picture-frame pattern).
Osteoporosis of aging. Generalized demineralization of the spine in a postmenopausal woman. The cortex appears as a thin line that is relatively dense and prominent (picture-frame pattern).
Anatomy on Thyroid sonography
The anterior neck is depicted rather well with standard gray scale sonography. (FIGURE 1) The thyroid gland is slightly more echo-dense than the adjacent structures because of its iodine content. It has a homogenous ground glass appearance. Each lobe has a smooth globular-shaped contour and is no more than 3 - 4 centimeters in height, 1 - 1.5 cm in width, and 1 centimeter in depth. The isthmus is identified, anterior to the trachea as a uniform structure that is approximately 0.5 cm in height and 2 - 3 mm in depth.
The pyramidal lobe is not seen unless it is significantly enlarged. In the female, the upper pole of each thyroid lobe may be seen at the level of the thyroid cartilage, lower in the male. The surrounding muscles are of lower echogenicity than the thyroid and tissue planes between muscles are usually identifiable. The air-filled trachea does not transmit the ultrasound and only the anterior portion of the cartilaginous ring is represented by dense, bright echoes. The carotid artery and other blood vessels are echo-free unless they are calcified. The jugular vein is usually in a collapsed condition and it distends with a Valsalva maneuver. There are frequently 1-2 mm echo-free zones on the surface and within the thyroid gland that represent blood vessels. The vascular nature of all of these echoless areas can be demonstrated by color Doppler imaging to differentiate them from cystic structures (10-11).
Lymph nodes may be observed and nerves are generally not seen. The parathyroid glands are observed only when they are enlarged and are less dense ultrasonically than thyroid tissue because of the absence of iodine. The esophagus may be demonstrated behind the medial part of the left thyroid lobe, especially if it is distended by a sip of water. (FIGURE 2)
The pyramidal lobe is not seen unless it is significantly enlarged. In the female, the upper pole of each thyroid lobe may be seen at the level of the thyroid cartilage, lower in the male. The surrounding muscles are of lower echogenicity than the thyroid and tissue planes between muscles are usually identifiable. The air-filled trachea does not transmit the ultrasound and only the anterior portion of the cartilaginous ring is represented by dense, bright echoes. The carotid artery and other blood vessels are echo-free unless they are calcified. The jugular vein is usually in a collapsed condition and it distends with a Valsalva maneuver. There are frequently 1-2 mm echo-free zones on the surface and within the thyroid gland that represent blood vessels. The vascular nature of all of these echoless areas can be demonstrated by color Doppler imaging to differentiate them from cystic structures (10-11).
Lymph nodes may be observed and nerves are generally not seen. The parathyroid glands are observed only when they are enlarged and are less dense ultrasonically than thyroid tissue because of the absence of iodine. The esophagus may be demonstrated behind the medial part of the left thyroid lobe, especially if it is distended by a sip of water. (FIGURE 2)
Figure 1. Sonogram of the neck in the transverse plane showing a normal right thyroid lobe and isthmus. L=small thyroid lobe in a patient who is taking suppressive amounts of L-thyroxine, I=isthmus, T=tracheal ring ( dense white arc is calcification, distal to it is artefact), C=carotid artery ( note the enhanced echoes deep to the fluid-filled blood vessel), J=jugular vein, S=Sternocleidomastoid muscle, m=strap muscle.
Figure 2. Sonogram of the left lobe of the thyroid gland in the transverse plane showing a rounded lobe of a goiter. L=enlarged lobe, I= widened isthmus, T=trachea, C=carotid artery ( note the enhanced echoes deep to the fluid-filled blood vessel), J=jugular vein, S=Sternocleidomastoid muscle, m=strap muscles, E=esophagus.
Complementary ultrasound to mammography ; Why?
Breast cancer can lie hidden from mammography in women with dense breast tissue, and thus the role of ultrasound is implemented to evaluate the texture and anatomical structures within the breast. Women most likely to have dense breasts are younger, premenopausal women and postmenopausal women who are taking hormone replacement therapy.
Breast ultrasound is used as a complementary examination to mammography in the following situations:
* Evaluation of dense breast tissue.
* Evaluation of a mass demonstrated on mammography.
* Guidance of biopsy needle or needle localization (see cyst aspiration image)
Breast ultrasound is used as a complementary examination to mammography in the following situations:
* Evaluation of dense breast tissue.
* Evaluation of a mass demonstrated on mammography.
* Guidance of biopsy needle or needle localization (see cyst aspiration image)
Grades of hydronephrosis (on Ultrasound imaging):
A) Mild hydronephrosis:
 This images shows mild dilatation of the pelvis as well as the calyces of the right kidney suggesting mild hydronephrosis. The left kidney also appears to be affected similarly. This must be differentiated from mild dilatation of the renal pelvis alone (called splitting of the pelvis), which is physiological and transient; this means that on emptying of the urinary bladder, this appearance should disappear.
This images shows mild dilatation of the pelvis as well as the calyces of the right kidney suggesting mild hydronephrosis. The left kidney also appears to be affected similarly. This must be differentiated from mild dilatation of the renal pelvis alone (called splitting of the pelvis), which is physiological and transient; this means that on emptying of the urinary bladder, this appearance should disappear.
B) Moderate hydronephrosis:

 The above ultrasound images show cupping of the calyces with moderate dilation (Right kidney) of the pelvis and calyces. Despite the hydronephrosis the renal parenchyma is still preserved.
The above ultrasound images show cupping of the calyces with moderate dilation (Right kidney) of the pelvis and calyces. Despite the hydronephrosis the renal parenchyma is still preserved.
C) Severe hydronephrosis:

 The above sonographic images show marked dilatation of the pelvicalyces with sever thinning of the renal parenchyma. note almost total absence of normal renal tissue (cortex).
The above sonographic images show marked dilatation of the pelvicalyces with sever thinning of the renal parenchyma. note almost total absence of normal renal tissue (cortex).
 This images shows mild dilatation of the pelvis as well as the calyces of the right kidney suggesting mild hydronephrosis. The left kidney also appears to be affected similarly. This must be differentiated from mild dilatation of the renal pelvis alone (called splitting of the pelvis), which is physiological and transient; this means that on emptying of the urinary bladder, this appearance should disappear.
This images shows mild dilatation of the pelvis as well as the calyces of the right kidney suggesting mild hydronephrosis. The left kidney also appears to be affected similarly. This must be differentiated from mild dilatation of the renal pelvis alone (called splitting of the pelvis), which is physiological and transient; this means that on emptying of the urinary bladder, this appearance should disappear.B) Moderate hydronephrosis:

 The above ultrasound images show cupping of the calyces with moderate dilation (Right kidney) of the pelvis and calyces. Despite the hydronephrosis the renal parenchyma is still preserved.
The above ultrasound images show cupping of the calyces with moderate dilation (Right kidney) of the pelvis and calyces. Despite the hydronephrosis the renal parenchyma is still preserved.C) Severe hydronephrosis:

 The above sonographic images show marked dilatation of the pelvicalyces with sever thinning of the renal parenchyma. note almost total absence of normal renal tissue (cortex).
The above sonographic images show marked dilatation of the pelvicalyces with sever thinning of the renal parenchyma. note almost total absence of normal renal tissue (cortex).
A case of Giant Left Atrium

An 83-year-old woman with long-standing atrial fibrillation who had previously undergone atrioventricular nodal ablation and pacemaker placement presented with symptoms of progressive heart failure.
Physical examination was notable for elevated jugular venous pressure, precordial lift, a grade 2/6 holosystolic murmur at the sternal border and apex, hepatomegaly, ascites, and severe lower-extremity edema.
Laboratory evaluation revealed a creatinine level of 1.4 mg per deciliter (124 µmol per liter), an albumin level of 3.6 g per deciliter, and a brain natriuretic peptide level of 526 pg per milliliter (normal range, 0 to 100 pg per milliliter); liver function was normal.
Chest radiography
An echocardiogram
An esophagogram
The patient was discharged home on medical management after prolonged diuresis.
Patient Preparation and Position for the Ultrasound Examination
Patient Preparation.
The ultrasound examination is most effective if the patient has been NPO for at least 6 hours. This allows the biliary system to be distended and easily imaged by the sonographer. When a patient is fasting there is a a decreased opportunity for gas to accumulate within the colon; gas prohibits the passage of the sound and thus limits visualization of abdominal structures. If the patient is able to consume liquids and the pancreas is not well-visualized, the administration of 32 oz. of water may be given to fill the stomach and duodenum to better delineate the pancreas.The kidneys are best imaged when the patient is fully hydrated, therefore no patient preparation is necessary when only the kidneys are examined. Full hydration will also enable the sonographer to image the distended urinary bladder.
Patient Position.
The position of the patient for the general abdominal scan is usually supine for the initial images. The patient is then rolled into various degrees of obliquity to better demonstrate the biliary system, pancreas, liver, kidneys, or spleen. If the scanning plane is oblique, the sonographer should indicate the change of position on the documented image without specifying the exact degree of obliquity. The same would apply if the patient were in a lateral, upright, or prone position.
Subscribe to:
Posts (Atom)
Popular Posts
-
W ind --- pneumonia, atelectasis at 1st 24- 48 hours W ater --- urinary tract infection at Anytime after post op day 3 W ound --- wound ...
-
Raccoon Eyes. Ecchymosis in the periorbital area, resulting from bleeding from a fracture site in the anterior portion of the skull base. Th...
-
Lymph Nodes : The major lymph node groups are located along the anterior and posterior aspects of the neck and on the underside of the jaw. ...
-
Fournier's gangrene is a rare condition and delayed treatment results in fatal outcome. We managed a case of Fournier's gangrene by...
-
Viewed posteriorly the right kidney has its upper edge opposite the 11th dorsal spine and the lower edge of the 11th rib. Its lower edge is ...
-
If you are palpating a swelling like an abdominal swelling infront of the aorta, You have to decide whether the mass you feel is pulsatile/e...
-
This raised skin lesion with a central necrotic area has the appearances of a keratoacanthoma. The natural history of these lesions is that...
-
The sphenoid bone carries its share of creating part of the base of the cranium. While it can be seen laterally and inferiorly, the shape of...