all you need to enjoy medicine. Daily medical Videos,Cases,Diagrams, Animation,Articles,Free medical books and news.
Criteria of growing pains
A 12-year-old obese boy presents to your office complaining of bilateral leg pain that occurs only at night. His mother denies any pain during the day and reports he has not had a limp. The most likely diagnosis is :
A) slipped capital femoral epiphysis
B) Legg-Calve-Perthes disease
C) Osgood Schlatter's disease
D) patellofemoral syndrome
E) growing pains
The answer is E.
A diagnosis of growing pains must meet three criteria:
(1) the leg pain is bilateral;
(2) the pain occurs only at night; and
(3) the patient has no limp, pain, or symptoms during the day.
To inaccurately diagnose a limping child with growing pains can be dangerous, as the physician risks missing the underlying pathology. However, if a child does fit the criteria for growing pains, the parents should be reassured that this is a benign, self-limited process that occurs for unknown reasons.
A) slipped capital femoral epiphysis
B) Legg-Calve-Perthes disease
C) Osgood Schlatter's disease
D) patellofemoral syndrome
E) growing pains
Answer and Discussion
The answer is E.
A diagnosis of growing pains must meet three criteria:
(1) the leg pain is bilateral;
(2) the pain occurs only at night; and
(3) the patient has no limp, pain, or symptoms during the day.
To inaccurately diagnose a limping child with growing pains can be dangerous, as the physician risks missing the underlying pathology. However, if a child does fit the criteria for growing pains, the parents should be reassured that this is a benign, self-limited process that occurs for unknown reasons.
Mottled skin or Cutis Marmorata in neonates
Cutis marmorata or "marbled skin" refers to mottled skin, typically in newborns in the first few months of life.
This reticulated pattern of constricted capillaries and venules is often called "mottling" due to vasomotor instability in immature infants. It generally resolves with increasing age and for most infants is of no significance.
In spite of it`s insignificance in most babies ,it may reflect underlying poor perfusion and infants who develop mottling and are unwell need to be clinically evaluated for sepsis and other illnesses.
It is localised , marked and more pronounced form of cutis marmorata which may be associated with other defects. It is uncommon and sometimes called (congenital generalized phlebectasia)
cutis marmorata telangiectatica congenita is often reported in association with a variety of other congenital anomalies, the most common anomaly associated is Body asymmetry.
This reticulated pattern of constricted capillaries and venules is often called "mottling" due to vasomotor instability in immature infants. It generally resolves with increasing age and for most infants is of no significance.
Explanation of cutis marmorata :
This phenomenon is caused by instability or immaturity of the nerve supply to the superficial capillary blood vessels in the skin. This causes the blood vessels in some regions of the skin to dilate, producing a red color of the skin, while other regions are contracting, producing pale skin.In spite of it`s insignificance in most babies ,it may reflect underlying poor perfusion and infants who develop mottling and are unwell need to be clinically evaluated for sepsis and other illnesses.
Cutis Marmorata Telangiectatica Congenita :
 |
Reticular skin lesions on the right arm of a 7-y girl |
cutis marmorata telangiectatica congenita is often reported in association with a variety of other congenital anomalies, the most common anomaly associated is Body asymmetry.
A case of Chromoblastomycosis
A 55-year-old man presented with vegetating lesions on the right foot that had been slowly enlarging during the past several years ;The photo:
On physical examination, several nodular and verrucous lesions were seen in the distal region of the foot. The patient lived in a rural area and had walked barefoot for most of his life. Analysis of a skin-biopsy specimen revealed clusters of small, round, thick-walled, brown sclerotic bodies in the stratum corneum (muriform cells), which are diagnostic for chromoblastomycosis.
Chromoblastomycosis is a chronic, soft-tissue fungal infection commonly caused by Fonsecaea pedrosoi, Phialophora verrucosa, Cladosporium carrionii, or F. compacta. The infection occurs in tropical or subtropical climates and often in rural areas. The fungi are usually introduced to the skin through cutaneous injury from thorns, splinters, or other plant debris. The patient was treated with multiple surgical excisions and itraconazole for 24 months with a complete resolution of symptoms.
On physical examination, several nodular and verrucous lesions were seen in the distal region of the foot. The patient lived in a rural area and had walked barefoot for most of his life. Analysis of a skin-biopsy specimen revealed clusters of small, round, thick-walled, brown sclerotic bodies in the stratum corneum (muriform cells), which are diagnostic for chromoblastomycosis.
Chromoblastomycosis is a chronic, soft-tissue fungal infection commonly caused by Fonsecaea pedrosoi, Phialophora verrucosa, Cladosporium carrionii, or F. compacta. The infection occurs in tropical or subtropical climates and often in rural areas. The fungi are usually introduced to the skin through cutaneous injury from thorns, splinters, or other plant debris. The patient was treated with multiple surgical excisions and itraconazole for 24 months with a complete resolution of symptoms.
Blood and nerve supply of a Synovial joint
The blood supply of a synovial joint is derived from the arteries sharing in the anastomosis around the joint.And the nerve supply of a synovial joint is derived from the muscles which act on the joint ,best expressed by Hilton in 1863:
"The same trunks of nerves, whose branches supply the groups of muscles moving a joint, furnish also a distribution of nerves to the skin over the insertions of the same muscles; and what at this moment more especially merits our attention-the interior of the joint receives its nerves from the same source."
proprioceptive fibers endings in the capsule and ligaments are very sensitive to position and movement. Their central connections are such that they are concerned with the reflex control of posture and locomotion and the detection of position and movement.
"The same trunks of nerves, whose branches supply the groups of muscles moving a joint, furnish also a distribution of nerves to the skin over the insertions of the same muscles; and what at this moment more especially merits our attention-the interior of the joint receives its nerves from the same source."
proprioceptive fibers endings in the capsule and ligaments are very sensitive to position and movement. Their central connections are such that they are concerned with the reflex control of posture and locomotion and the detection of position and movement.
The blood and nerve supply of a synovial joint. This diagram shows the artery supplying the epiphysis, joint capsule, and synovial membrane. The nerve that contains (1) sensory (mostly pain) fibers from the capsule and synovial membrane, (2) autonomic (postganglionic sympathetic) fibers to blood vessels, (3) sensory (pain) fibers from the adventitia of blood vessels, and (4) proprioceptive fibers.
N.B.Arrowheads indicate direction of conduction.
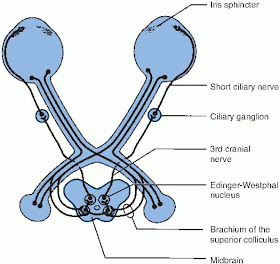
Diagram shows pathway of the pupillary light reflex
This is a schematic diagram of the pupillary light reflex. The afferent limb originates in the retinal photoreceptors, which convert light energy to a neural signal. Pupillary information is conveyed from the eye to the brain by the melanopsin-expressing retinal ganglion cells, and their axons project to the dorsal midbrain, synapsing in the pretectal olivary nucleus. Each pretectal olivary nucleus distributes the afferent pupillary impulses to the ipsilateral and contralateral Edinger-Westphal subnucleus of the oculomotor nuclear complex.
The neurons of the Edinger-Westphal subnucleus initiate the efferent limb of the pupillary light reflex, that is, pupilloconstriction. Efferent pupillomotor impulses travel in the parasympathetic fibers of the oculomotor nerve, synapse in the ciliary ganglion of the orbit, and then pass via the short ciliary nerves to innervate the iris sphincter muscle.
The neurons of the Edinger-Westphal subnucleus initiate the efferent limb of the pupillary light reflex, that is, pupilloconstriction. Efferent pupillomotor impulses travel in the parasympathetic fibers of the oculomotor nerve, synapse in the ciliary ganglion of the orbit, and then pass via the short ciliary nerves to innervate the iris sphincter muscle.
Causes of osteoporotic changes in Cushing’s syndrome
Patients with Cushing’s syndrome often show osteoporotic changes.Which of the following is involved in the etiology of osteoporosis induced by Cushing’s syndrome?
Osteoporosis may also be induced by other diseases (e.g., hyperthyroidism) or drugs (e.g., alcohol and caffeine). In addition, excess glucocorticoid induces osteoporosis. For example, in Cushing’s syndrome, patients produce high levels of corticosteroids that interfere with bone metabolism. A similar pattern may be seen during prolonged steroid therapy. The result is increased bone resorption compared with bone deposition. Intestinal calcium absorption is inhibited and PTH "Parathormone" levels may be increased.
- a.Decreased glucocorticoid levels that result in decreased quality of the bone
- deposited
- b.Excess deposition of osteoid
- c.Stimulation of intestinal calcium absorption
- d.Decreased PTH levels
- e.Bone fragility resulting from excess bone resorption
The answer is E.
Osteoporosis is a major problem of normal aging in both sexes but is particularly prevalent in older women. In that disease, the quality of bone is unchanged, but the balance between bone deposition and bone resorption is lost. The disease is prevalent in postmenopausal women because the protective effect of estrogens is no longer present. Osteoporosis may also be induced by other diseases (e.g., hyperthyroidism) or drugs (e.g., alcohol and caffeine). In addition, excess glucocorticoid induces osteoporosis. For example, in Cushing’s syndrome, patients produce high levels of corticosteroids that interfere with bone metabolism. A similar pattern may be seen during prolonged steroid therapy. The result is increased bone resorption compared with bone deposition. Intestinal calcium absorption is inhibited and PTH "Parathormone" levels may be increased.
Botox injections into the bladder
A short video demonstration injections of diluted Botulinum toxin "Botox"into the bladder.
The operation takes approximately 10 minutes and is done as a day-case procedure. It is usually well tolerated under local anaesthesia, but for some women a general anaesthetic may be the preferred option. A very fine needle is inserted into the bladder through a cystoscope , and the diluted Botulinum toxin is then injected into 15-20 sites in the bladder wall.
This treatment is suitable for women with severe urgency, frequency, and urge-incontinence that is unresponsive to other treatment, such as bladder retraining and medications.
The operation takes approximately 10 minutes and is done as a day-case procedure. It is usually well tolerated under local anaesthesia, but for some women a general anaesthetic may be the preferred option. A very fine needle is inserted into the bladder through a cystoscope , and the diluted Botulinum toxin is then injected into 15-20 sites in the bladder wall.
This treatment is suitable for women with severe urgency, frequency, and urge-incontinence that is unresponsive to other treatment, such as bladder retraining and medications.
Skin manifestations of Pellagra
Pellagra is a a vitamin deficiency disease caused by chronic lack of nicotinic acid (niacin, vitamin B3) or its precursor, tryptophan.Niacin is required for most cellular processes.
• Alcoholism, malabsorption, anorexia nervosa, Prolonged diarrhoea, Liver cirrhosis, Drugs e.g. isoniazid, azathioprine
• Carcinoid tumors (excessive use of tryptophan, which produces serotonin)
Symptoms and signs of Pellagra is classically described by "the four D's": diarrhea, dermatitis, dementia and If left untreated, death.
-The rash is usually symmetrical with a clear edge between affected and unaffected skin and sometimes may be itching or burning sensation
-Other features sometimes present include cheilosis, glossitis, angular stomatitis, and oral or perianal sores.
CAUSE of Pellagra:
Inadequate niacin and/or tryptophan in the diet mainly seen in developing countries or poverty stricken areas "called Primary pellagra".But usually there is something prevents Niacin absorption and processing and causes secondary pellagra such as:• Alcoholism, malabsorption, anorexia nervosa, Prolonged diarrhoea, Liver cirrhosis, Drugs e.g. isoniazid, azathioprine
• Carcinoid tumors (excessive use of tryptophan, which produces serotonin)
Symptoms and signs of Pellagra is classically described by "the four D's": diarrhea, dermatitis, dementia and If left untreated, death.
Skin manifestations and clinical finding of Pellagra:
-At first there is reddened skin with superficial scaling in areas exposed to sunlight, heat & friction. This may resemble severe sunburn then gradually subsides leaving a dusky brown-red colouration .-The rash is usually symmetrical with a clear edge between affected and unaffected skin and sometimes may be itching or burning sensation
-Other features sometimes present include cheilosis, glossitis, angular stomatitis, and oral or perianal sores.
Legs and feet of a patient with niacin deficiency. A, Before therapy. B, After therapy.
(From Swartz MH: Textbook of Physical Diagnosis, 5th ed. Philadelphia, WB Saunders, 2006.)
TREATMENT of Pellagra:
• Nutritional supplementation with niacin will improve the appearance of skin lesions
Gross and Microscopic picture of Renal Infarction
1- Gross specimen of Renal infarction:
The kidney is cut in half along its longitudinal axis, exposing :
(A.) the cortex
(B.) the medulla
(C.) a minor calyx .
The pyramidal shaped infarct is pale as compared to the adjacent normal cortex. Why? as the wedge shape of this zone of coagulative necrosis resulting from loss of blood supply with resultant tissue ischemia that produces the pale infarct.
The arrow points to a line of hyperemia that represents the interface between normal and necrotic tissue.
2- Microscopic section of Renal infarction:
* The thick arrow points to glomerulus in an area of coagulation (ischemic) necrosis.
* The thin arrow points to a glomerulus which is in the interface between necrotic and normal kidney.
The kidney is cut in half along its longitudinal axis, exposing :
(A.) the cortex
(B.) the medulla
(C.) a minor calyx .
The pyramidal shaped infarct is pale as compared to the adjacent normal cortex. Why? as the wedge shape of this zone of coagulative necrosis resulting from loss of blood supply with resultant tissue ischemia that produces the pale infarct.
The arrow points to a line of hyperemia that represents the interface between normal and necrotic tissue.
2- Microscopic section of Renal infarction:
* The thick arrow points to glomerulus in an area of coagulation (ischemic) necrosis.
* The thin arrow points to a glomerulus which is in the interface between necrotic and normal kidney.
Psoriasis photo affects the elbows
A 45-year-old woman presents with a localized area of erythematous scaly patches that comes and goes and typically affects the elbows. The likely diagnosis is.........
- A) pityriasis rosacea
- B) mycosis fungoides
- C) tinea corpora
- D) nummular eczema
- E) psoriasis
The answer is E. (Psoriasis)
Psoriasis usually manifests itself as erythematous scaly patches that affect the knees or elbows. More severe cases can involve multiple areas over the entire body. Extensor surfaces are predominantly affected. Nail pitting may be present. The condition appears to be hereditary. Diagnosis is usually based on clinical findings. Skin biopsy may be helpful for definitive diagnosis. Treatment consists of topical steroids, intralesional steroids, tar preparations, anthralin, tazarotene, and calcipotriene.
ALCOHOL as Teratogen :Fetal Alcohol Syndrome
In many countries alcohol is the Most common teratogen.And the severity of spectrum of effects in the neonate correlates with the amount of alcohol consumed , ranging from mild reduction in cerebral function to classic fetal alcohol syndrome .
* Palpebral fissure - short opening of eye
* Epicanthal folds - fold of skin at inside of corner of eye
* Midface - flat
* Nasal Bridge - low
* Philtrum - Indistinct, vertical grooves between nose and mouth
* Upper Lip - thin
* Micrognathia - small jaw
* Ears - curve at top part of outer ear is underdeveloped and folded over parallel to curve beneath. Gives the appearance of a "railroad track"
It also associated with :
#Mild to severe mental retardation resulting in learning difficulties.
#Low birth weight and height that persists through early childhood.
#Abnormalities of the heart and other organs.
Fetal Alcohol Syndrome. Notice the depressed nasal bridge, flat philtrum, long upper lip, and thin vermillion border.
Facial features of Fetal Alcohol Syndrome (FAS)
* Microcephaly - leads to small head circumference* Palpebral fissure - short opening of eye
* Epicanthal folds - fold of skin at inside of corner of eye
* Midface - flat
* Nasal Bridge - low
* Philtrum - Indistinct, vertical grooves between nose and mouth
* Upper Lip - thin
* Micrognathia - small jaw
* Ears - curve at top part of outer ear is underdeveloped and folded over parallel to curve beneath. Gives the appearance of a "railroad track"
It also associated with :
#Mild to severe mental retardation resulting in learning difficulties.
#Low birth weight and height that persists through early childhood.
#Abnormalities of the heart and other organs.
Fetal Alcohol Syndrome. Notice the depressed nasal bridge, flat philtrum, long upper lip, and thin vermillion border.
Why cricothyrotomy is the best site for emergency airway
You witness a choking incident in a restaurant. The Heimlich maneuver is unsuccessful at removing the food from the pharynx. The victim is having extreme difficulty breathing and starts to pass out. Where are you most likely to produce an emergency airway?
Locations around the hyoid bone (answers a and b)and above the laryngeal notch (answer c)are above the blockage and would not get air into the lungs. The isthmus of the thyroid gland
generally lies in front of the second and third tracheal ring (answer e), and because it is so highly vascular, it is not an ideal location for an emergency airway.
An additional alternative location for an emergency airway would be the jugular notch, but is not preferred because of the occurrence of a thyroid ima artery below the isthmus, in a small percentage of the population.
- a.In the midline just superior to the hyoid bone
- b.In the midline just inferior to the hyoid bone
- c.At the laryngeal notch
- d.At the junction between the thyroid cartilage and cricoid cartilage
- e.At tracheal ring 2 to 3 below the cricoid cartilage
The answer is (d).
The food is most likely stuck in the laryngeal pharynx, so you must produce an alternative airway below the glottis, which reflexly closes.Locations around the hyoid bone (answers a and b)and above the laryngeal notch (answer c)are above the blockage and would not get air into the lungs. The isthmus of the thyroid gland
generally lies in front of the second and third tracheal ring (answer e), and because it is so highly vascular, it is not an ideal location for an emergency airway.
An additional alternative location for an emergency airway would be the jugular notch, but is not preferred because of the occurrence of a thyroid ima artery below the isthmus, in a small percentage of the population.
More useful links :
Perforation of Nasal Septum
Etiology of nasal septal perforations can be classified into these 4 main categories: traumatic, iatrogenic, inflammatory/malignant, and cocaine use.
Most traumatic or iatrogenic perforations result from mucosal lacerations on corresponding sides of the septum with exposure of the underlying cartilage or from a fracture of the cartilaginous septum. Perforation occurs because the cartilage relies upon the overlying mucoperichondrium for its blood supply and nutrients.
Iatrogenic causes include nasal surgical procedures (prior septal surgery is the most common cause of septal perforations) and nasal intubation or nasogastric tube placement.
Septal hematoma, if not identified and treated early, also may result in perforation.
Infectious and inflammatory etiologies, including tuberculosis, syphilis, Wegener granulomatosis, and sarcoidosis, always should be considered in the differential diagnosis.
Treatment involves the use of nasal wetting agents, placement of a plastic button over the perforation, and surgical repair. Repair with surgery is very difficult and failure to close the perforation is common.
Notes on gallbladder stones
The photo below shows multiple faceted gallstones that can be composed of either cholesterol, bile pigments or a mixture of the two.
-Pigment stones are often small and occur in patients with either congenital or acquired haemolytic states (5%).
-Cholesterol stones are often large and solitary (15%).
The stones shown are mixed stones and account for approximately 80% of all gallstones.
"Mixed stones are probably a variant of cholesterol stones"
Only 10% of gallstones are symptomatic.Also about 10% of gallstones are radio-opaque and visible on a plain abdominal film.
-Pigment stones are often small and occur in patients with either congenital or acquired haemolytic states (5%).
-Cholesterol stones are often large and solitary (15%).
The stones shown are mixed stones and account for approximately 80% of all gallstones.
"Mixed stones are probably a variant of cholesterol stones"
Pathophysiology:
Cholesterol stones result from a change in solubility of bile constituents- Bile acids act as a detergent keeping cholesterol in solution
- Bile acids, lecithin and cholesterol result in the formation of micelles
- Bile is often supersaturated with cholesterol
- This favours the formation of cholesterol microcrystals
- Biliary infection, stasis and changes in gallbladder function can precipitate stone formation
Only 10% of gallstones are symptomatic.Also about 10% of gallstones are radio-opaque and visible on a plain abdominal film.
Magnesium sulfate as the drug of choice for controlling eclamptic seizures
The drug of choice for controlling eclamptic seizures is
- A) hydralazine
- B) phenobarbital
- C) phenytoin
- D) diazepam
- E) magnesium sulfate
Answer and Discussion
The answer is E.
In the United States, magnesium sulfate is considered the drug of choice for controlling eclamptic seizures. Fewer intubations are required in the neonates of eclamptic women who are treated with magnesium sulfate. In addition, fewer newborns require placement in neonatal intensive care units. In the treatment of eclampsia and preeclampsia, magnesium sulfate is often given according to established protocols. If serum magnesium levels exceed 10 mEq/L (5 mmol/L), respiratory depression can occur. This problem may be counteracted by the rapid intravenous infusion of 10% calcium gluconate. Magnesium sulfate should be used with caution in patients with impaired renal or cardiac status. It should not be used in patients with myasthenia gravis.
Mnemonic for Malignant hyperthermia treatment
Malignant hyperthermia or malignant hyperpyrexia is a rare life-threatening condition that is usually triggered by exposure to certain drugs used for general anesthesia in the operating room or also occur within the first few hours of recovery from anesthesia; specifically, the volatile anesthetic agents and the neuromuscular blocking agent, succinylcholine.
The syndrome is though to be due to a reduction in the reuptake of calcium by the sarcoplasmic reticulum necessary for termination of muscle contraction. Consequently, muscle contraction is sustained, resulting in signs of hypermetabolism, including acidosis, tachycardia, hypercarbia, glycolisis, hypoxemia, and heat production (hyperthermia).
Remember
"Some Hot Dude Better Give Iced Fluids Fast!"
(Hot dude = hypothermia):Stop triggering agents
Hyperventilate/ Hundred percent oxygen
Dantrolene (2.5mg/kg)
Bicarbonate
Glucose and insulin
IV Fluids and cooling blanket
Fluid output monitoring/ Furosemide/ Fast heart [tachycardia]
Barrett's esophagus
The Key word :
BARRett's = Becomes Adenocarcinoma, Results from Reflux.
Barrett's esophagus is a Glandular metaplasia ,or replacement of non keratinized (stratified) squamous epithelium with intestinal (columnar) epithelium in the distal esophagus as a serious uncommon complication of chronic acid reflux or GERD (gastroesophageal reflux disease) .
 By endoscope :
By endoscope :
the color and composition of the tissue lining the lower esophagus change. Instead of pink, the tissue turns a salmon color.
Under a microscope, the tissue resembles that of the small intestine "metaplasia".
This Metaplasia is brought on by repeated and long-term exposure to stomach acid and is associated with an increased risk of esophageal cancer.
BARRett's = Becomes Adenocarcinoma, Results from Reflux.
Barrett's esophagus is a Glandular metaplasia ,or replacement of non keratinized (stratified) squamous epithelium with intestinal (columnar) epithelium in the distal esophagus as a serious uncommon complication of chronic acid reflux or GERD (gastroesophageal reflux disease) .
 By endoscope :
By endoscope :the color and composition of the tissue lining the lower esophagus change. Instead of pink, the tissue turns a salmon color.
Under a microscope, the tissue resembles that of the small intestine "metaplasia".
This Metaplasia is brought on by repeated and long-term exposure to stomach acid and is associated with an increased risk of esophageal cancer.
ECG of Supraventricular tachycardia
A 36-year-old white female nurse comes to the ER due to a sensation of fast heart rate, slight dizziness, and vague chest fullness. Blood pressure is 110/70. The following rhythm strip is obtained, which shows which of the following?
Atrial fibrillation would show an irregularly irregular rhythm without discrete P waves. Wide QRS complexes with rate greater than 100 would be expected in ventricular tachycardia.
- a.Atrial fibrillation
- b.Atrial flutter
- c.Supraventricular tachycardia
- d.Ventricular tachycardia
The answer is (c).
Paroxysmal supraventricular tachycardia due to AV nodal reentry typically displays a narrow QRS complex without clearly discernible P waves, with a rate in the 160 to 190 range. The atrial rate is faster in atrial flutter, typically with a classic sawtooth pattern of P waves, with AV conduction ratios most commonly 2:1 or 4:1, leading to ventricular rates of 150 or 75 per min. Atrial fibrillation would show an irregularly irregular rhythm without discrete P waves. Wide QRS complexes with rate greater than 100 would be expected in ventricular tachycardia.
Insulin injection lipodystrophy
Many patients whit type 1 diabetes mellitus may presented with depressed areas of skin at the sites of insulin injection due to lipoatrophy......!!
Lipodystrophy or lipoatrophy is a recognized complication of Insulin injection due to loss of the adipose tissue layer at the sites of injection (prevalence of 3.6%).
The pathogenesis remains unknown, but possible mechanisms include immune reaction to insulin or excipients of the injection solution, injury from cold insulin, or trauma from repeated local injections.
Lipodystrophy or lipoatrophy is a recognized complication of Insulin injection due to loss of the adipose tissue layer at the sites of injection (prevalence of 3.6%).
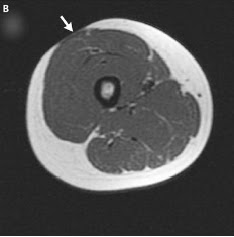
Axial magnetic resonance imaging of the right thigh showed Lipoatrophy of a 14-year-old girl with a 20-month history of type 1 diabetes mellitus
The pathogenesis remains unknown, but possible mechanisms include immune reaction to insulin or excipients of the injection solution, injury from cold insulin, or trauma from repeated local injections.
Common recommended sites for insulin injection
At first insulin recommended to be injected into some sites where a less-sensitive layer of fatty tissue just below the skin to absorb the insulin with no many nerves ,so that insulin injection will be more comfortable in these sites more than others the just under the skin.
Also these sites make it easier to inject into the subcutaneous tissue, where insulin injection is recommended.
B-Thighs :The middle and outer thigh area is another one of the common insulin injection sites that are suitable for injecting long-acting insulin.Don't inject too close to the area just above knee because the tissue is very tough.
C-Arms :The back of the upper arm
Also these sites make it easier to inject into the subcutaneous tissue, where insulin injection is recommended.
Common sites for insulin injection are :
A-Abdomen :the most common insulin injection site because it has easily accessible fatty areas and Insulin is absorbed faster when it is injected into the abdomen " So:you should inject the insulin into the abdomen just before meals",Also This area allows for greater access if injecting individually. Notes:
Do not inject within 1-2 inches around the navel "tissue is tough" ,surgical, other scar tissue, moles.B-Thighs :The middle and outer thigh area is another one of the common insulin injection sites that are suitable for injecting long-acting insulin.Don't inject too close to the area just above knee because the tissue is very tough.
C-Arms :The back of the upper arm
Primary sclerosing cholangitis
Primary sclerosing cholangitis (PSC) is a chronic liver disease characterized by cholestasis ,caused by progressive inflammation and scarring of the bile ducts of the liver. This inflammation impedes the flow of bile to the gut, which can ultimately lead to liver cirrhosis, liver failure and liver cancer.
The underlying cause of the inflammation is still unknown, but a variety of factors are thought to be involved. An autoimmune mechanism is suggested, since approximately 75-90% of patients with PSC have inflammatory bowel disease (IBD).
The left image shows a histologic specimen demonstrating chronic inflammation surrounding the bile duct.
The gross specimen ,the right picture demonstrates the thickening of the wall of the bile duct (arrow) causing many strictures.
Note that the strictures in PSC are short in the order of 3-5 mm in length, which is helpful to remember because if you are looking for cholangiocarcinoma, the malignant strictures usually exceed 10 mm in length.
The underlying cause of the inflammation is still unknown, but a variety of factors are thought to be involved. An autoimmune mechanism is suggested, since approximately 75-90% of patients with PSC have inflammatory bowel disease (IBD).
The left image shows a histologic specimen demonstrating chronic inflammation surrounding the bile duct.
The gross specimen ,the right picture demonstrates the thickening of the wall of the bile duct (arrow) causing many strictures.
Note that the strictures in PSC are short in the order of 3-5 mm in length, which is helpful to remember because if you are looking for cholangiocarcinoma, the malignant strictures usually exceed 10 mm in length.
(ERCP) Endoscopic retrograde cholangiopancreatography of the patient showed intra- and extrahepatic bile-duct strictures (thin arrow) and dilations (thick arrow).
Photos of Pectus Excavatum (Funnel chest)
Definition :
Congenital posterior displacement of lower aspect of sternum.This gives the chest a somewhat "hollowed-out" appearance. Pectus Excavatum is one of the most common congenital deformity of the chest wall "The condition is more common than Down syndrome".in Pectus Excavatum several ribs and the sternum grow abnormally, producing a concave, or caved-in, appearance in the anterior chest wall and a displaced heart which is often palpable on the left mid-axillary line slightly below the armpit.
-Pectus Excavatum is sometimes also called sunken chest or funnel chest.
-Pectus excavatum occurs more often in males than females (3:1) ,some studies say that this ratio reached 6:1 ,and accounts for 90% of congenital chest wall deformities.
Pathogenesis :
pathogenesis of pectus excavatum still unclear, and, to date, no known genetic defect is directly responsible for the development of pectus excavatum despite of familial occurrence of pectus deformity that reported in 35% of cases, investigators have hypothesized that the deformity results from unbalanced overgrowth in the costochondral regions.in other words; an abnormality of connective tissue (cartilage) sometimes associated with Marfan and Ehlers Danlos syndromes.The "Nuss" procedure or pectum bar operation, This operation involves the placement of a customized, long, curved metal bar under the sternum. Two small incisions are made on each side of the chest to allow insertion of the bar. Another small incision is made to insert a thoracoscope, which allows us to watch the bar as it goes under the sternum. The bar is secured to the ribs on the side of the chest and pushes the sternum forward. Neither the rib cartilages nor sternum are cut. The bar usually remains in place for two years and is then removed with a second, smaller operation. The principle of the pectus bar operation is that the rib cartilage remodel while the bar is in place--similar to the remodeling of the mouth with orthodonture.
Skeletal System Structures and Functions
An overview of the functions and structures of the skeletal system.
Carbon monoxide poisoning in 20-year old fireman
A 20-year-old fireman comes to the emergency room complaining of headache and dizziness after helping to put out a garage fire. He does not complain of shortness of breath, and the arterial blood gas shows a normal partial pressure of oxygen. Which of the following is the best first step in the management of this patient?
The use of supplementary oxygen prior to obtaining the test may be a confounding factor in interpreting blood levels. Oxygen or even hyperbaric oxygen is given after blood for carboxyhemoglobin is drawn.
Chest x-ray should also be obtained. It may be normal or show a pattern of nonpulmonary edema, or aspiration in severe cases. Central nervous system imaging would not be indicated, and there are no diagnostic patterns that are specific to carbon monoxide poisoning.
- a.Begin oxygen therapy
- b.Obtain chest x-ray
- c.Obtain carboxyhemoglobin level
- d.Obtain CT scan
The answer is c.
With symptoms of headache and dizziness in a fireman, the diagnosis of carbon monoxide poisoning must be addressed quickly. A venous or arterial measure of car-boxyhemoglobin must first be obtained, if possible, before oxygen therapy is begun. The use of supplementary oxygen prior to obtaining the test may be a confounding factor in interpreting blood levels. Oxygen or even hyperbaric oxygen is given after blood for carboxyhemoglobin is drawn.
Chest x-ray should also be obtained. It may be normal or show a pattern of nonpulmonary edema, or aspiration in severe cases. Central nervous system imaging would not be indicated, and there are no diagnostic patterns that are specific to carbon monoxide poisoning.
Subcuticular (or Intradermal) Suturing
Demonstration of subcuticular or intradermal suturing technique for wound closure in the operating room.
Hoover sign Explanation in COPD case
At first you should know that there are 2 signs named for Charles Franklin Hoover :
1-Hoover's sign of leg paresis.
2-Hoover’s sign in pulmonology which we will take about ;
It refers to inward movement of the lower rib cage during inspiration, implying a flat, but functioning, diaphragm, often associated with COPD.
COPD, and more specifically emphysema, often lead to hyperexpansion of the lungs due to air trapping. The resulting flattened diaphragm contracts inwards instead of downwards, thereby paradoxically pulling the inferior ribs inwards with its movement.

1-Hoover's sign of leg paresis.
2-Hoover’s sign in pulmonology which we will take about ;
It refers to inward movement of the lower rib cage during inspiration, implying a flat, but functioning, diaphragm, often associated with COPD.
COPD, and more specifically emphysema, often lead to hyperexpansion of the lungs due to air trapping. The resulting flattened diaphragm contracts inwards instead of downwards, thereby paradoxically pulling the inferior ribs inwards with its movement.

This case for A 70-year-old man with a 70 pack-year history of smoking was referred to the emergency department for an exacerbation of chronic obstructive pulmonary disease (COPD).
On examination, he breathed through pursed lips and had paradoxical indrawing of the lower rib cage margin with inspiration (Hoover sign)(Figure 1A),A chest radiograph showed distension of the lungs and flattening of the diaphragm(Figure 1B).
See this video:
How to do Vertical Mattress Suturing ?
Demonstration of vertical mattress suturing technique for laceration repair or wound closure in the operating room.
How to do Horizontal Mattress Suturing ?
Demonstration of horizontal mattress suturing technique for laceration repair or wound closure in the operating room.
Classic description of Normal-pressure hydrocephalus
A 75-year-old man is brought in to your office by his wife. She complains that he is not the same over the last 6 months. His memory is failing him, he has difficulty walking (especially when he initiates walking), and he is incontinent of urine. Which of the following is the most likely diagnosis based on his history?
NPH classically consists of dementia, apraxia of gait, and incontinence, but many patients with these symptoms do not have NPH. Typically, motor weakness and staggering are absent, but initiation of gait is hesitant—described as a “slipping clutch” or “feet stuck to the floor” gait—and walking eventually occurs. NPH has also been associated with various psychiatric manifestations that are not categorical. NPH should be considered in the differential diagnosis of any new mental status changes in the elderly.
CT or MRI and a lumbar puncture are necessary for diagnosis. On CT or MRI, the ventricles are dilated. CSF pressure measured by a lumbar puncture is normal. A limited improvement after removing about 50 mL of CSF indicates a better prognosis with shunting. Radiographic or pressure measurements alone do not seem to predict response to shunting. Shunting CSF from the dilated ventricles sometimes results in clinical improvement, but the longer the disease has been present, the less likely shunting will be curative.
- A) Alzheimer's disease
- B) Parkinson's disease
- C) Normal-pressure hydrocephalus
- D) Pick's disease
- E) Progressive supranuclear palsy
The answer is (C).
Normal-pressure hydrocephalus (NPH) is a cause of dementia in the elderly. It may be caused by previous insult to the brain, usually as a result of a subarachnoid hemorrhage or diffuse meningitis that presumably results in scarring of the arachnoid villi over the brain convexities where cerebrospinal fluid (CSF) absorption usually occurs. However, elderly NPH patients seldom have a history of predisposing disease.NPH classically consists of dementia, apraxia of gait, and incontinence, but many patients with these symptoms do not have NPH. Typically, motor weakness and staggering are absent, but initiation of gait is hesitant—described as a “slipping clutch” or “feet stuck to the floor” gait—and walking eventually occurs. NPH has also been associated with various psychiatric manifestations that are not categorical. NPH should be considered in the differential diagnosis of any new mental status changes in the elderly.
CT or MRI and a lumbar puncture are necessary for diagnosis. On CT or MRI, the ventricles are dilated. CSF pressure measured by a lumbar puncture is normal. A limited improvement after removing about 50 mL of CSF indicates a better prognosis with shunting. Radiographic or pressure measurements alone do not seem to predict response to shunting. Shunting CSF from the dilated ventricles sometimes results in clinical improvement, but the longer the disease has been present, the less likely shunting will be curative.
5 Steps to Chest X-ray Interpretation
The video shows some basics of chest x-ray interpretation. From ed4nurses.com
Diagram of Anterior anatomical relations of both kidneys
The kidneys are retroperitoneal organs that are located in the perirenal retroperitoneal space with a longitudinal diameter of 10–12 cm and a latero-lateral diameter of 3–5 cm and a weight of 250–270 g.
In the supine position, the medial border of the normal kidney is much more anterior than the lateral border, The upper pole of each kidney is situated more posteriorly than the lower pole.
The right kidney, anteriorly :
has a relation with the inferior surface of the liver with peritoneal interposition,and with the second portion of the duodenum without any peritoneal interposition since the second portion of the duodenum is retroperitoneal .
The left kidney, anteriorly :
has a relation with the pancreatic tail, the spleen, the stomach, the ligament of Treitz and small bowel, and with the left colic lexure and left colon . Over the left kidney, there are two important peritoneal relections, one vertical corresponding to the spleno-renal ligament (connected to
the gastro-diaphragmatic and gastrosplenic ligaments) and one horizontal corresponding to the transverse mesocolon.
In the supine position, the medial border of the normal kidney is much more anterior than the lateral border, The upper pole of each kidney is situated more posteriorly than the lower pole.
The right kidney, anteriorly :
has a relation with the inferior surface of the liver with peritoneal interposition,and with the second portion of the duodenum without any peritoneal interposition since the second portion of the duodenum is retroperitoneal .
The left kidney, anteriorly :
has a relation with the pancreatic tail, the spleen, the stomach, the ligament of Treitz and small bowel, and with the left colic lexure and left colon . Over the left kidney, there are two important peritoneal relections, one vertical corresponding to the spleno-renal ligament (connected to
the gastro-diaphragmatic and gastrosplenic ligaments) and one horizontal corresponding to the transverse mesocolon.
Picture of Cranial Nerve 12 (Hypoglossal Nerve XII) Dysfunction and Assessment
Hypoglossal nerve is a motor cranial nerve for the muscles of the tunge.So,If the right CN 12 is dysfunctional, the tongue will deviate to the right. This is because the normally functioning left half will dominate as it no longer has opposition from the right. Similarly, the tongue would have limited or absent ability to resist against pressure applied from outside the left cheek.
•If there is any suggestion of deviation to one side/weakness, direct them to push the tip of their
tongue into either cheek while you provide counter pressure from the outside.
This photo shows Cranial Nerve 12 Dysfunction: Stroke has resulted in loss of function of left CN 12. When patient sticks tongue out, it therefore deviates to the left.
Assessment is performed as follows:
•Ask the patient to stick their tongue straight out of their mouth.•If there is any suggestion of deviation to one side/weakness, direct them to push the tip of their
tongue into either cheek while you provide counter pressure from the outside.